By Joanne P. Shelby-Klein BSN RN
 The shingles vaccine, sometimes referred to as the ‘shingles shot’ is often seen advertised in pharmacies and Doctors’ offices, leading patients to wonder if they should get the vaccine and what is it for. Shingles is the layman’s term for the Herpes Zoster Virus and the vaccine is used prevent the shingles from occurring.
The shingles vaccine, sometimes referred to as the ‘shingles shot’ is often seen advertised in pharmacies and Doctors’ offices, leading patients to wonder if they should get the vaccine and what is it for. Shingles is the layman’s term for the Herpes Zoster Virus and the vaccine is used prevent the shingles from occurring.
WHAT IS THE HERPES ZOSTER VIRUS?
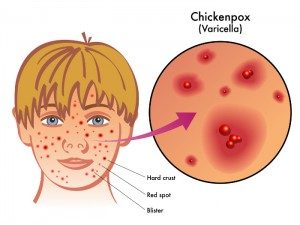
Herpes Zoster is the same virus that causes chicken pox, the varicella-zoster virus also known as the human herpes virus type 3. Chicken pox is known as the active invasive form of the virus, while the shingles comes from the dormant virus that suddenly becomes activated.
Scientists believe that when a person has chicken pox parts of the virus go into a dormant or inactive state in the neural ganglia in the spinal column and brain and remain there for years causing no problems until the virus suddenly re-activates and creates an active infection along the sensory portion of the involved ganglia.
HOW COMMON ARE THE SHINGLES?
95% of adults and 99.5% of people over the age of 40 in the United States carry the dormant shingles virus and are vulnerable to it becoming active and a full blown infection. It is important to remember that anyone of any age who has had the chicken pox virus is at risk for reactivation of the virus, the risk of it happening increases with age.
WHO’S AT RISK FOR GETTING THE SHINGLES?
- People who are over the age of 60
- People who had chicken pox before their first birthday
- People who have a disease that weakens the body’s immune system
- People who are on medications that slow down or suppress the immune system
- People who have had bone marrow or organ transplants
- Men and women are equally at risk.
- Black people have a lower risk of getting shingles than do white people. The reason for this is unknown.
WHAT CAN RE-ACTIVATE THE VIRUS?
What causes the virus to be re-activated is not fully known and understood at this time. The following are believed to be some reasons why it happens:
In extremely rare cases the herpes zoster virus may cause the patient to have meningitis or encephalitis. These patients will complain of headache, fever, seizures and change in mental status and when the spinal tap is performed the herpes virus is found in the culture.
IS THE SHINGLES CONTAGIOUS?
The herpes zoster virus can be spread from a person who has singles to a person who has never had chicken pox, putting them at risk for getting chicken pox, not the shingles. The virus spreads when a person comes in direct contact with the fluid filled blisters on the rash.
This means a person with shingles is considered contagious when they are in the blister phase. Before the blisters appear and after they crust over, the person is no longer considered contagious. People who have shingles need to:
- Make sure the rash is covered with a loose, natural fiber cloth or clothing.
- Try not to scratch the rash. If the itch is severe, contact your healthcare provider for suggestions.
- Wash hands often, using a liquid soap and paper towels to dry.
- Avoid contact with any pregnant women who have not had the chicken pox vaccine and any prematurely born babies.
- Stay away from people who have immune systems that are weak because of illness or medications.
HOW ARE SHINGLES TREATED?
Children who develop the shingles usually have it resolve without any medical treatments. For adults the treatment way depend on the symptoms and their severity as well as any other medical conditions they may have.
- Non-steroidal anti-inflammatory medications such as Ibuprofen
- Moist dressings to the rash area using a 5% aluminum acetate solution
- Calamine lotion for the itch.
Some patients may require hospitalization and additional more aggressive treatments.
- Steroids to help with the inflammation
- Analgesics or pain medication to help relieve the pain and discomfort
- Anti-viral medications such as Acyclovir. Anti-virals can help shorten the length of time for the blisters to appear and crust over. Anti-virals can be taken by mouth and to be most effective, need to be started within 72 hours of the appearance of the first symptoms. The medication may be given for 7-21 days.
DOES SHINGLE CAUSE LONG-TERM COMPLICATIONS?
Healthcare providers are always concerned when a patient comes in with shingles because there is a risk of the patient developing Postherpatic Neuralgia or PHN. PHN is defined as any pain that occurs 1 month to 6 months after the shingles rash is noticed. This pain can last for months or years after the rash and other symptoms have gone. It can be very difficult to treat. The goal of all healthcare providers is to treat the virus promptly and aggressively to prevent PHN from happening.
Studies show that the older the patient is, the greater the risk for PHN. One study showed that in patients who had pain for greater than 90 days, the PHN rate increasing as follows based on age:
- 5% in patients under 60 years of age
- 10% in patients between 60 – 69 years
- 20% in patients over the age of 80
PHN pain is often described as being intermittent and comes on suddenly, without warning or a precipitating cause and usually comes as a result of damage to the sensory nerves. Areas of the skin that usually are not sensitive to painful stimuli seem to be the most affected areas.
Patients who have PHN often say that the slightest touch or brush of cloth is painful and that their sleep and daily activities are changed. The persistent pain often leads to depression.
IS THERE ANY TREATMENT AVAILABLE FOR POSTHERPATIC NEURALGIA (PHN)?
There is no one single treatment that effectively treats PHN. Most treatments involve the use of topical medications that go directly on the skin as well as medication that is taken by mouth and into the blood stream.
Some of the topical agents include:
- Lidocaine patches that serve as a protective barrier from clothing and rubbing. They also help by slowing down the small nerve fiber activities and lessening the pain.
- Capsaicin cream has also been shown in research studies to be safe and effective in minimizing the pain, especially when used for 4 weeks or more. When the cream is first used it can cause a strong burning sensation. This burning sensation will go away after a few uses.
Medications taken by mouth:
- Antidepressants have been shown in research studies to be the most effective for relieving the pain caused by PHN. It may take some trial and error to find the antidepressant that works without causing the patient to be drowsy or sedated.
- Anticonvulsants or anti-seizure medication. These medications have proven effective in treating severe nerve or neuropathic pain. Neurontin also known as Gabapentin is the most commonly prescribed medication.
- Opioid based pain medications can be used to help relieve the pain, especially for the elderly. These medications include Tramadol, Oxycodone, and even Morphine.
CAN SHINGLES BE PREVENTED?
The Food and Drug Administration approved a vaccine for in shingles in 2006. This vaccine, Zostavax, contains a live version of the virus that is found in the chicken pox vaccine given to children. The vaccine is approved for use in people over the age of 60, although it can be given to people between the age of 50 and 59 if deemed necessary by a healthcare provider.
Keep in mind that the chicken pox vaccine came out for general use in 1995, 11 years before the shingles vaccine became available. When the shingles vaccine came out in 2006 there was no one over the age of 60 who had been vaccinated against the chicken pox or shingles.
Zostavax does not cure shingles once the virus becomes active. It is given as an injection and only one dose is needed. People who are pregnant, thinking of becoming pregnant, taking high doses of steroids or immunosuppressant medication or are allergic to neomycin should not get the vaccine. People who are going to receive the vaccine should be off any immunosuppressive medications for a minimum of 14 days, preferably one month, before receiving the injection.
IS THE SHINGLES VACCINE EFFECTIVE?
Studies have been done to determine the safety and effectiveness of the vaccine. One study was a double-blind placebo controlled study that involves 38,000 adults age 60 or older. This study showed that the vaccine
- Lowered the number of occurrences of shingles by 51%
- Lessened the patient burden of the illness by 61%
- Lessened the risk of PHN by 60%
- The vaccine was most effective between the ages of 60-69 years of age
- The vaccine was effective during the 4 year follow-up period
Another study was conducted over a 2 year period from January 2007 to December 2009 in 766,330 people ages 65 and older, representing a 5% random sample of people on Medicare. The results are as follows:
- The vaccine uptake rate was 3.9%, a low number with 0.3% rate noted in blacks and 0.5% in low income individuals.
- 13.112 developed shingles
- Shingles incident rate was 10.0 infections in a 1000 person years in the unvaccinated group and 5.4 infections per 1000 person years in those who received vaccines.
- Patients who were immunocompromised had less active infections when they were vaccinated.
- In the general population over the age of 65, a decrease in shingles infections and PHN was seen when the people received the vaccine.
IS THE VACCINE COVERED BY INSURANCE?
The vaccine is fairly expensive usually costing a minimum of $160.00. If a patient has a Medicare Part D program and is over the age of 65, it will be covered as a prescription drug. A co-pay may still apply and be billed to the patient since Medicare Part D does not cover the injection in full. The healthcare provider may also charge a vaccine administration fee that is not covered by insurance. It is important to talk with the healthcare provider and insurance company before getting the injection.
REFERENCES:
- Schmader, K. Gnann, JW,JR. Watson,CP. (2008, March). The epidemiological, clinical, and pathological rationale for the herpes zoster vaccine. J Infect Dis. 2008 Mar 1;197 Suppl 2:S207-15. doi: 10.1086/522152.
- Oxman MN1, Levin MJ; Shingles Prevention Study Group. Vaccination against Herpes Zoster and Post herpetic Neuralgia. J Infect Dis. 2008 Mar 1;197 Suppl 2:S228-36. doi: 10.1086/522159.
- Sampathkumar, P., Drage, L. A., & Martin, D. P. (2009). Herpes Zoster (Shingles) and Postherpetic Neuralgia. Mayo Clinic Proceedings, 84(3), 274–280.
- Langan, SM. Smeeth, L. Margolis, DJ. Thomas, SL. Herpes Zoster Vaccine Effectiveness against Incident Herpes Zoster and Post-herpetic Neuralgia in an Older US Population: A Cohort Study. Published: April 9, 2013 DOI: 10.1371/journal.pmed.1001420
- Janniger, CK, MD. Elston, DM. (2015, September). Herpes Zoster. Retrieved rom URL: http://emedicine.medscape.com/article/1132465-overview
- Ogle, KT, PhD, RN, FNP-BC. (2012, April) Shingles Made Easy. Nursing Made Incredibly Easy! -Feature Journal. August 2012, Volume 10 Number 4 , p 28 – 34
- Surlis, WD,MD. Santoro, J MD. Herpes Zoster Vaccine. Merck Manual Professional Edition. Retrieved from URL: http://www.merckmanuals.com/professional/infectious-diseases/immunization/herpes-zoster-vaccine
- Kaye, KM, MD. Herpes Zoster (Shingles; Acute Posterior Ganglionitis). Merch Manual Professional Edition. Retrieved from URL: http://www.merckmanuals.com/professional/infectious-diseases/herpesviruses/herpes-zoster
Hi there! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us valuable information to work on. You have done a
outstanding job!
Could you inform me what style are you making
use of on your site? It looks nice.