 [icon name=”user” class=”” unprefixed_class=””] Dr. Neerja L. Bisht
[icon name=”user” class=”” unprefixed_class=””] Dr. Neerja L. Bisht
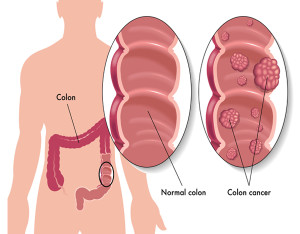
The colon and rectum form the large intestine in the human body. Unnatural growths or tumors that grow in the lining of the large intestine are termed as colorectal cancers. Colorectal cancers (CRCs) are common among both men and women. The risk of developing CRC rises after age 50, and is one of the leading causes of death from cancer in most countries.1Hence, it is important to know the various risk factors for developing CRC.
Risk factor
Most CRCs start as polyps, which are small growths (adenomas) that can be present for at least 10 years before they turn malignant (cancerous). The following factors play a role in developing CRC.2
- Family history of CRC
- Past history of carcinoma or an adenoma
- Inflammatory bowel disease: ulcerative colitis, Crohn’s colitis
- Polyposis syndromes
- Hereditary non-polyposis colorectal cancer (HNPCC).
- Hormonal factors: nulliparity, late age at first pregnancy, early menopause
- Diet: rich in red meat and fat; poor in fibre, folate and calcium
- Sedentary lifestyle, obesity, smoking, high alcohol intake
- Diabetes mellitus
- Previous irradiation, occupational hazards (asbestos exposure, etc.)
- Past history of small bowel cancer, endometrial cancer, breast cancer or ovarian cancer
Symptoms and Diagnosis
Colorectal cancer is locally invasive, and may not produce any symptoms even after spread (metastasis) has occurred. Usually, CRC spreads to the liver. Some symptoms have been recognized according to the site of the cancer: Right-sided CRCs are accompanied by weight loss, anaemia, occult bleeding, mass in right abdomen, disease more likely to be advanced at presentation; Left-sided CRCs are more likely to produce colicky pain, rectal bleeding, bowel obstruction, tenesmus (need to pass motion), mass in left abdomen, early change in bowel habit, less advanced disease at presentation.Patients with the following criteria must seek urgent medical care3:
- Aged 40 years and older with presence of a rectal bleed, with a change of bowel habit towards looser stools and/or increased stool frequency persisting for six weeks or more
- Aged 60 years and older, with presence of a rectal bleed for six weeks or more without a change in bowel habit and without anal symptoms
- Aged 60 years and older, with a change in bowel habit to looser stools and/or more frequent stools persisting for six weeks or more without rectal bleeding
- Any age with a right lower abdominal mass consistent with involvement of the large bowel
- Men of any age with unexplained iron-deficiency anaemia and a Hb of 11 g/100 ml or below
- Non-menstruating women with unexplained iron-deficiency anaemia and a Hb of 10 g/100 ml or below
Investigations
All patients must have a thorough abdominal and rectal examination. The presence of jaundice suggests advanced disease and spread to the liver.
- Colonoscopy should be offered to patients to confirm the diagnosis of CRC. If a lesion suspicious of cancer is detected, a biopsy sample for confirmation is sent. Sometimes, a flexible sigmoidoscopy is also used as an alternative to colonoscopy
- CT colonography can detect CRC; however, tissue diagnosis from the colonoscopy, the gold standard,is regarded as the final diagnosis
- Elevated pre-treatment serum levels of carcinoembryonic antigen (CEA) levels are tested, and high levels indicate disease prognosis. CEA levels are very useful in predicting relapse in patients after surgery suitable for further resection
Prevention recommendations
Cancer guidelines recommend screening for CRC starting at the age of 50, until the age of 75 years.4Persons with risk factors need to be screened earlier and more frequently to detect the presence of early disease. The following tests are recommended:
- High-sensitivity fecal occult blood test (FOBT) : checks for hidden blood in three consecutive stool samples; to be done every year.
- Flexible sigmoidoscopy : to look at the interior walls of the rectum and part of the colon; should be done every five years with FOBT every three years
- Colonoscopy : to be done every 10 years. In this procedures polyps can be visualized, if present, and removed
Screening recommendations with family history of CRC
The American College of Gastroenterology recommends the following5:Single first-degree relative (defined as mother, father, daughter, son, sister, brother) with CRC or advanced adenoma (adenoma >=1 cm in size, or with high-grade dysplasia or villous elements) diagnosed at age >=60 years.
- Recommended screening: same as average risk (colonoscopy every 10 years beginning at age 50 years)
Single first-degree relative with CRC or advanced adenoma diagnosed at age <60 years or two first-degree relatives with CRC or advanced adenomas.
- Recommended screening: colonoscopy every 5 years beginning at age 40, or 10 years younger than age at diagnosis of the youngest affected relative
Management of CRC
Once a diagnosis of CRC is confirmed, the tumor is staged by pathologybywhich the extent of cancer is can be determined. This is done through the tissue biopsy of a suspicious lesion during colonoscopy or during surgical resection of the tumor itself through surgery. Staging in CRC is also done by the TNM classification, as with other cancers. In CRC, T will denote how much of the tumor has invaded the walls of the intestine, or nearby areas; N will denote if the tumor has spread to the lymphatic nodes; and, M will indicate metastasis, or spread to other organs of the body. Numbers accompany each of the TNM classification from 0-4. The higher these numbers are, more severe is the disease.Once TNM staging is determined, the cancer can be grouped in Roman numerals I-IV, according to severity. Once again, stage IV represents advanced cancer. It is best to discuss you staging with your healthcare professional.Surgical options for colon cancer1: The type of surgery depends on the early or late cancers.
Polypectomy and local excision
Colonoscopy can find early cancers. Stage 0-1 cancers can remove the entire tumor and a bit of the surrounding normal tissue. Through colposcopy, polyps can also be located and excised at the stem.
Colectomy
Abdominal surgery is needed when all or part of the colon and lymph nodes need to be removed. Usually, the entire colon may not be needed to be removed. If the abdomen is opened up through a mid-line incision, it is called an open colectomy. The colon can be reached using a laparoscope through a tube to which a camera is attached for visualization. The main advantage of this type of surgery is that the hospital stay is much shorter compared to the open-type colectomy. Since special skills are required to insert and resect the tumor, only expert and experienced surgeons can tackle this procedure.
Abdominal surgery requires bowel preparation consisting of strong laxatives and an enema to completely empty the bowel. This enables the surgeon to visualize the interior of the colon better. If a part of the colon is removed, the procedure is called partial colectomy. The surgeon will also remove nearby lymph nodes (12 is recommended). Then the two cut ends of the colon are reattached.
Sometimes the ends of the colon are not attached and the upper end is connected to an abdominal opening called the stoma to allow the body waste matter out. This is known as a colostomy and is usually temporary. Similarly, sometimes the end of the small intestine (the ileum) is connected to a stoma in the skin instead of the colon. This is called an ileostomy. For either of these procedures, a removable collecting bag is connected to the stoma to hold the waste. This is no longer necessary when a colostomy reversal or ileostomy reversal surgery is carried out when the two ends of the colon are reattached inside the abdomen. In some cases, the colostomy or ileostomy may need to be permanent.
- Diverting colostomy
Some tumors can block the colon, and have possibly spread to other organs. In such cases instead of tackling the tumor, the colon is cut above the cancer and connected to a stoma. Then the patient can shrink the tumor with additional treatment such as radiotherapy or chemotherapy.
Surgery for colon cancer spread depends on size, location and number of organs to which it has spread. The affected colon and rectum is removed, and if the spread is limited only to a few areas, in the lungs or liver, they can also be removed to increase survival.
Surgery for CRC is a major surgery. Your doctor will advise the possible side-effects of the surgery and a person’s general health is an important factor in early recuperation. The most feared post-operative complication is when the ends of the attached colon inside the abdomen get infected and leak. The abdominal scar itself can open up delaying healing. After surgery, internal scarring can cause tissues or organs to stick together causing adhesions and block the bowel that might once again require surgery
Colostomy
Getting used to colostomy takes some time to get used to. Certain lifestyle adjustments will help in leading a life as close to before the procedure. Specially trained ostomy nurses can help in the immediate post-operative period, and guide to choosing and managing the best pouch system. Home nursing facilities are also offered to some patients.Unlike passing bowels through the anus, which can control bowel movement with a sphincter, ostomas do not have any control over bowel movements. Some patients can regulate their bowel movements with changes in their diets. This can eliminate gas and odor to some degree. Maintaining a food diary by jotting the foods that suit the body and ones that don’t is very helpful. Most pouch systems are now odor-free and waterproof. This makes bathing and swimming easy. While changing the base to which the pouch is attached, the skin can be sore. Changing the base and leaving it to dry before applying the base can help heal the redness associated with the glue/adhesive of the base. It is also important to maintain a clean stoma. Colostomies are sometimes associated with hernia, blockage, and infections.
Contact your doctor immediately, if there is bleeding, watery/pus discharge, bulge and no output from stoma.
Surgical options for rectal cancer : The type of surgery depends on the early or late cancers
Surgery is usually the main treatment for rectal cancer, although radiation and chemotherapy will often be given before or after surgery to shrink the tumor size.
- Polypectomy and local excision
These procedures are essentially the same as for colon cancers for early small rectal cancers. Some centers are equipped with special equipment that can carry out microsurgeries.
- Low anterior resection
This procedure is done for upper end rectal cancers that are close to the lower end of the colon, so when the tumor is removed, the colon is attached to the lower end of the rectum and the anus which is spared.This way, after the surgery, bowel movement is normal.
- Proctectomy with colo-anal anastomosis
Some cancers involve most of the rectum, so the entire rectum is removed. This procedure is called a proctectomy. The healthy colon end is then connected to the anus, known as colo-anal anastomosis.
- Abdominoperineal resection (APR)
This operation will involve tackling the cancer in the rectum, but the anus is also removed. This will require a permanent colostomy.
- Pelvic exenteration
This type of surgery is carried out when nearby organs are also involved in the spread of the rectal cancer.The bladder and prostate in men or the uterus in women are often affected. In case the bladder is removed, in addition, a urostomy will also be needed this is an opening for collection of urine.This will be in addition to a colostomy.
References:
- Available at: http://nihseniorhealth.gov/colorectalcancer/colorectalcancerdefined/ 01.html. Accessed 01-06-2015.
- Available at: http://patient.info/doctor/colorectal-cancer. Accessed on 01-06-2015.
- Available at: http://www.cancer.org/cancer/colonandrectumcancer/moreinformation/ colonandrectumcancerearlydetection/colorectal-cancer-early-detection-acs-recommendations. Accessed 06-06-2015.
- Available at:http://www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/colorectal-cancer-screening Accessed 01-06-2015.
- Available at:http://gi.org/guideline/colorectal-cancer-screening/Accessed 09-06-2015.
- Available at: http://www.cancer.org/cancer/colonandrectumcancer/detailedguide. Accessed 09-06-2015.