Carol Yu, Ph.D.
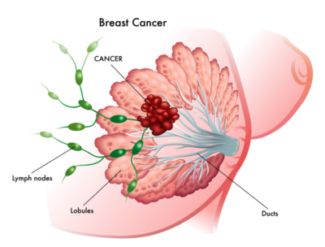
Breast cancer is the most common cancer in women worldwide, and is a disease in which cancer cells form in breast tissues that are mainly made up of lobes and ducts. In the United States, breast cancer accounts for 29% for all different types of cancers in women [1]. According to the World Health Organization, it was estimated that over 50,8000 women worldwide died in the year of 2011 from breast cancer (Global Health Estimates, WHO 2013), and an estimated 40,290 women in the United States will die from breast cancer in 2015 (American Cancer Society). Primarily a disease affecting women, men account for less than 1% of breast cancer cases and deaths [2]. The number of breast cancer cases has been increasing since the 1970s due to widespread adoption of breast cancer screening, mammography and post-menopausal hormone therapy [3, 4].
Breast cancer is a rather broad disease, meaning that there are many types of disease sub-types with different features and clinical behavior. The most common type of breast cancer is called ductal carcinoma, which begins in the ducts of the breast tissues. On the other hand, Inflammatory Breast Cancer, in which there is swelling of the breast tissues, is an uncommon type of breast cancer. There are 4 stages of breast cancer, which will be discussed later.
In terms of survival, the earlier stage the breast cancer is at, the better chances of survival it is for the patient. As well, there is generally a trend for greater survival chances when the tumor is small in size and/or does not involve much of lymph nodes [5]. As a result, early detection of breast cancer is important for the best breast cancer treatment outcome. Because of the differences in availability of early detection programs around the world, there are variable survival rates worldwide. For example, in low-income countries, survival rates are below 40%, while it is around 60% in middle-income countries and over 80% in high-income countries [6].
Risk factors are anything that would increase chances of getting a disease, and in this case, breast cancer. However, having a certain risk factor does not mean that you will get breast cancer, and vice versa. The incidence of breast cancer is increasing in the developing world primarily due to increased life expectancy [7], urbanization and adaptation to the western lifestyles [8].
- family history of breast cancer [9]
- certain high-risk genes (e.g. BRCA1, BRCA 2, Her 2)inherited from your parents [10–12]
- increasing age [12]
- alcoholic intake [12–14]
- high mammographic densities in the breasts (meaning more epithelial and stromal tissues in relation to fat tissues) [15]
- obesity [16]
- lack of exercise [14, 17]
- taking oral contraceptives [18]
- early-age menstruation and late-age menopause [12]
- never having given birth or giving birth at older age [12]
- breast/chest exposure to radiation [19]
Screening tests:
These include the annual mammograms (X-ray of breasts), breast MRI, ultrasound exam to provide early detection of breast cancer before symptoms can develop.
Diagnostic tests:
if you are suspected to have breast cancer, a biopsy test may be done to determine presence of breast cancer and stage of cancer. Some diagnostic tests may also include a chest X-ray, CT scan, and a bone-scan.
Monitoring tests:
These tests are used after the diagnosis of breast cancer. They are used to monitor how well the patient is responding to the treatment, and to see if there are any recurrences.
Once you have been diagnosed with breast cancer, tests are done to see if cancer cells have spread within the breast (metastatic breast cancer) and/or to other parts of the body. Whether the cancer has spread and how much it has spread will determine which stage the cancer is at. It is important for physicians to decide the strategy of treatment depending on the stage of breast cancer.
Stage 0
This stage is called “carcinoma in situ”. At this stage, there are abnormal cells in a breast duct but these cells are not spread to any nearby tissues.
Stage I
This is early stage breast cancer. The tumour is not more than 2 centimeters across.
Stage II
At this stage, the breast cancer is growing but is contained in the breast or nearby lymph nodes. Stage II is further categorized into Stage IIA and IIB depending on the size of the tumour and whether it has spread to nearby lymph nodes.
Stage III
The breast cancer has spread beyond the original region of the tumour into surrounding lymph nodes and muscles, but not to distant organs. This stage is further categorized into Stage IIIA, IIIB, and IIIC according to the size of the tumour and how much it has spread to the surrounding lymph nodes and muscles.
Stage IV
This is advanced stage breast cancer (Metastatic Breast Cancer). At this stage, the cancer is considered invasive and has spread to other areas of the body such as the brain, the lungs, and the liver. Although this stage has been considered incurable, recent advances in breast cancer research and development have led to recent treatments that extended lives of many women [20].
Breast cancer, like any other types of cancer, can spread via the tissue itself, the lymph system, and blood.
Through the tissue itself, cancer can spread from its original growth area to nearby areas. Through the lymph system, cancer spreads from its original area into the lymph systems and the cancer travels through lymph vessels to other parts of the body. Through the circulation system, or blood, cancer spreads by getting into the blood and travels to other parts of the body. The process of cancer spreading from where it begins to other parts of the body is called metastasis.
BREAST CANCER TREATMENT OPTIONS:
Breast cancer treatment options for the patients depend on a number of factors including:
- the stage of breast cancer
- the type of breast cancer
- how fast the tumour is growing
- how likely the tumour will come back
- the patient’s age, menopausal status, and health status
Some of the most common treatments used in breast cancer patients will first be explained, followed by their practices according to each stage of cancer.
This method uses cancer-killing drugs by either injecting the drug intravenously (into the vein) or by mouth. The drugs get into the bloodstream to reach cancer cells throughout the body. Often times, a combination of drugs is used for more effective results. Some common drugs used to treat breast cancer will be outlined in a later section.
This method relies on high-energy rays to kill cancer cells and this method only affects the cells in the area that are directly treated. Sometimes, radiation therapy may be used after surgery to kill remaining cancer cells.
If your lab tests from your breast tissues indicate that your breast cancer cells contain hormone receptors, hormone therapy may be an option for you. This type of treatment includes drugs to treat breast cancer that is hormone-sensitive. This treatment also includes surgery to remove the ovaries. However, tumors that are smaller than 1 centimeter across are less likely to benefit from hormone therapy.
Lumpectomy refers to a surgery in which only the tumour and some of the surrounding tissues are removed. Often times, lumpectomy is followed by radiotherapy to give an appealing alternative to mastectomy.
This combination of techniques was pioneered in the early 1970s in the United States describing successful rates of disease control and cosmetic results [21, 22].
Mastectomy may be used to remove one or both breasts, partially or completely, and is dependent on stage and feature of cancer, location of breast cancer, size of breasts, and the feasibility of alternative radiotherapy. Breast reconstruction, which is a plastic surgery to rebuild the breast, is an option after mastectomy.
Stage 0:
Surgery is standard as a treatment option for breast cancer at this stage. If the tumour is small enough, a lumpectomy will be performed to remove only the abnormal cells and only some breast tissues will be removed. Some may choose to have mastectomy, which is remove the whole breast. Afterwards, plastic reconstruction is a possible option post-surgery. Sometimes after either surgery, radiation or hormone therapy may serve as additional means to decrease risks of another breast cancer occurrence.
Stage I:
Because the cancers are relatively small still, and have not spread to nearby lymph nodes, local therapy are used for treatment at this early-stage. Breast-conserving surgery or mastectomy is used and usually followed by radiation therapy to lower the chance of cancer recurrence, similar to patients faced with Stage 0 breast cancer. However, older patients typically over the age of 70 may consider opting out of radiation therapy if the tumour has been completely removed, hormone therapy is given, and lymph nodes removed from surgery do not contain cancer. Sometimes chemotherapy with cancer drugs may be used before surgery in the attempt shrink the tumour size so that a less extensive surgery can be performed.
Stage II:
Surgery to remove the breast, or mastectomy, and/or breast-conserving surgery are commonly used to treat Stage II breast cancer. Hormone therapy, chemotherapy, and radiotherapy are options of treatment after surgery, similar to Stages 0 and I. Also similar to early stages, chemotherapy to decrease tumour size may be used before the surgery.
Stage III:
Chemotherapy using anticancer drugs is common as a treatment option at this stage. Hormone therapy is also used for breast cancers that are sensitive to this type of therapy. For some women, surgery, either lumpectomy or mastectomy, will be used to remove the tumour and surrounding tissues from the breast. For larger tumours, chemotherapy before surgery will be used. Often times, radiation therapy is practised after surgery to ensure remaining cancer cells are destroyed. At this stage, physicians consider a number of different treatment options and their combinations depending on the particular breast cancer case and patient. Women can also consider new clinical trails that are taking place for the most current clinical options.
Stage IV:
At this stage, the cancer is metastatic, meaning that it has spread beyond its original site. Similar to Stage III, the physician and the patient can consider a number of options, including chemotherapy, radiation therapy, surgery, hormone therapy, and/or clinical trials. At this stage, focused treatment using only one treatment option is likely not sufficient to treat the breast cancer. As well, if the breast cancer is diagnosed at this stage, treatment does not provide a cure for the disease, but will delay the progression of the cancer.
Outcomes for breast cancer vary largely depending on the cancer type, patient’s age, and stage of the disease. Survival rates are typically used by doctors to talk to their patients about the prognosis or outlook. A 5-year survival rate refers to the percentage of patients who live more than 5 years after being diagnosed with cancer. For patients diagnosed with Stages 0 or I, the 5-year survival rate is 100%. For those diagnosed with Stage II, it is 93%; Stage III, it is 72%, and at Stage IV, it is 22%. (Data from the National Institute’s SEER database).
Patients who go through surgery to treat breast cancer commonly experience pain, tenderness, and tight skin tissues around the area where surgery is performed. In addition, arm, shoulder, neck, and back muscles may experience weakness and stiffness. To manage these symptoms, talk to your healthcare team to discuss the plan for pain relief, such as using pain medication.
For those who go through radiation therapy as a treatment option or an additional treatment option, it is common for the treated skin area to become dry, tender, red, itchy, and there may be permanent color change in that area. The use of lotion or cream recommended by your healthcare team can be used to manage these side effects. Wearing loose clothing during this time can also prevent clothing fabric to rub against your skin. Fatigue is also a common side effect, and studies have shown that higher levels of physical functions such as participating in walking exercise programs can help manage fatigue during radiation therapy for cancer patients [23].
If you are treated with hormone therapy, some common side effects can be hot flashes, vaginal discharge, and nausea.
Because of its high prevalence, breast cancer is well studied in terms of its psychological and psychosocial aspects. Diagnosis of breast cancer and its treatment are major stressors for women and have major psychological impacts on their emotions [24, 25]. Emotional support through supportive group intervention as well as improved relationships with family and friends can result in psychological benefit for breast cancer patients [26], and may reduce anxiety [27], although it may not prolong survival in women with early-stage breast cancer [28].
There are many approved drugs out there on the market, and doctors typically give cancer drugs in cycles so that there is recovery time for the patient between cycles of drugs used. Schedules of drugs given and length of drug cycles depend on the particular drug(s) used, and should be well explained to you by your doctor.
As there are many different types of drugs on the market that are used to treat breast cancer at different stages, only some of the more common drugs used will be presented below to identify their uses or benefits as well as their known side-effects.
Doxorubicin
Under the trade name Adriamycin, doxorubicin targets cancer cell growth by interfering with their DNA. The most serious adverse effect of using this drug is heart damage, which can be life threatening. Another serious adverse effect that can also be life threatening is inflammation of the bowel system. Other less serious side effects include possible hair loss, myelosuppression, nausea and vomiting, oral mucositis, esophagitis, diarrhoea, skin reactions, and local swelling (where drug is administered).
Epirubicin
Under the trade name Ellence or Pharmorubicin, epirubicin are used in breast cancer patients after undergoing surgery. These drugs act by interfering cancer cell DNA, thus slowing tumour growth. This drug is sometimes favoured over doxorubicin because of its fewer life-threatening adverse effects. Still, some documented side effects include nausea and vomiting, diarrhoea, unusual fatigue, stomach pain, loss in appetite, mouth/throat sores, and hair loss.
Paclitaxel:
The trademark for this drug is Taxol, and is used to treat breast cancer by interference of cancer cell division, and thus repressing tumour growth. Some of the common side effects are fever, chills, cough, sore throat, hair loss, loss in appetite, unusual bruising or bleeding, diarrhoea, muscle/joint pains, local swelling, chest pain, increased risk for infections, and sometimes infertility. When used during pregnancy, problems in the baby have been reported.
Docitaxel:
With the trade name Taxotere or Docecad, these drugs also work by interference of call cell division. Hair loss and blood cell abnormalities are some of the common side effects associated with the use of docitaxel.
Fluorouracil
Trademarked as Adrucil, Carac, Efudex and Efudix, these drugs act by interrupting DNA replication, thus stopping tumour cell growth. There are many reported side effects associated with the use of fluorouracil, including nausea, vomiting, mood disorders, hiccups, itchiness, diarrhoea, mucositis, headache, hair loss, myelosuppression, swelling or numbness in the palm and feet. A more serious adverse effect related to drug is damages in the nervous system.
Capecitabine
With the trade name Xeloda, capecitabine works similarly to fluorouracil and has common side effects including loss in appetite, fatigue, nausea, vomiting, indigestion, fever, headache, loss in hearing, abdominal pain, shortness of breath, eye irritation, and bone marrow suppression.
Cyclophosphamide
Also known as cytophosphane, with trade names Endoxan, Cytoxan, Revimmune, Cyclobastin, Neosar, and Procytox, these drugs interfere with DNA replication. Chemotherapy with this drug has been linked to serious adverse effects, such as acute myeloid leukemia, permanent infertility, and bladder cancer. Other less severe side effects are nausea and vomiting, bone marrow suppression, diarrhoea, hair loss, stomach ache, lower urinary tract symptoms, fatigue, joint pain, mouth sores, unusual bruising and bleeding, and discolour or skin and nails.
Carboplatin
Under the trade names Paraplatin and Paraplatin-AQ, carboplatin is used in chemotherapy to interfere with cancer cell DNA repair, thus interfering tumour growth. A great benefit of this drug is its small number of side effects, although still include bone marrow suppression, nausea and vomiting.
Trastuzumab
Traded as Herceptin or Herclon, trastuzumab is used in hormone therapy to treat hormone-sensitive breast cancer. This drug interferes cell-cell communication to eliminate cancer cell growth. While it has been shown to reduce risk of cancer recurrence, it is associated with adverse effects such as heart damages. Other common side effects include fever, chills, nausea, and diarrhoea.
Pertuzumab
Also known as 2C4, traded under the name Perjeta, this drug is also used in hormone therapy to treat hormone-sensitive breast cancer, and is used to slow tumour growth. Commonly used in combination with trastuzumab and docetaxel, side effects with this drug include heart damages, diarrhoea, nausea, vomiting, fatigue, hair loss, and loss of appetite. It may also cause fatal effects to a fetus if it is used during pregnancy.
Cisplatin
This chemotherapy drug, like many other drugs, triggers cancer cell death. Side effects with the use of this drug include kidney damages, nerve damages, loss in hearing, bone marrow suppression, hair loss, nausea, and vomiting.
Vinorelbine
With the trade name Navelbine, this anti-tumour drug inhibits cancer cell growth. Possible side effects include pain and numbness in the arms and legs, bruising and bleeding, decreased resistance to infection, fatigue, constipation, diarrhoea, nausea, and vomiting.
Gemcitabine
Marketed as Gemzar, this drug arrests tumour growth by disrupting DNA replication. Some side effects with the use of this drug include fever, chills, fatigue, nausea and vomiting, loss of appetite, diarrhoea, hair loss, shortness of breath, mouth sores, and hair loss.
Mitoxantrone
With the trade name Novantrone, it is often used to treat advanced-stage breast cancer. The use of mitoxantrone can cause side effects ranging from hair loss, nausea and vomiting, to heart damages and immunosuppression.
Ixabepilone
With the trade name Ixempra, this drug can damage cancer cells in at a very low dose and has demonstrated effectiveness in treating advanced breast cancer. However, as with all other drugs, there are side effects associated with the use of this drug. They include fatigue, muscle or joint pain, nausea, vomiting, hair loss, loss of appetite, diarrhoea, and constipation.
Eribulin
Under the trade name Halaven, this anticancer drug is commonly used to treat advanced breast cancer by inhibiting cancer growth and thus killing them. Common adverse effects are hair loss, fatigue, headache, muscle or joint pain, nausea, vomiting, loss of appetite, and constipation.
- Siegel, R., et al., Cancer statistics, 2014. CA Cancer J Clin, 2014. 64(1): p. 9-29.
- Landis, S.H., et al., Cancer statistics, 1998. CA Cancer J Clin, 1998. 48(1): p. 6-29.
- Johnson, R.H., F.L. Chien, and A. Bleyer, Incidence of breast cancer with distant involvement among women in the United States, 1976 to 2009. JAMA, 2013. 309(8): p. 800-5.
- Johnson, A. and J. Shekhdar, Breast cancer incidence: what do the figures mean? J Eval Clin Pract, 2005. 11(1): p. 27-31.
- Carter, C.L., C. Allen, and D.E. Henson, Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer, 1989. 63(1): p. 181-7.
- Coleman, M.P., et al., Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Oncol, 2008. 9(8): p. 730-56.
- Porter, P., “Westernizing” women’s risks? Breast cancer in lower-income countries. N Engl J Med, 2008. 358(3): p. 213-6.
- Stoll, B.A., Western nutrition and the insulin resistance syndrome: a link to breast cancer. Eur J Clin Nutr, 1999. 53(2): p. 83-7.
- Colditz, G.A., B.A. Rosner, and F.E. Speizer, Risk factors for breast cancer according to family history of breast cancer. For the Nurses’ Health Study Research Group. J Natl Cancer Inst, 1996. 88(6): p. 365-71.
- Goodwin, P.J., et al., Breast cancer prognosis in BRCA1 and BRCA2 mutation carriers: an International Prospective Breast Cancer Family Registry population-based cohort study. J Clin Oncol, 2012. 30(1): p. 19-26.
- Mavaddat, N., et al., Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers: results from the Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA). Cancer Epidemiol Biomarkers Prev, 2012. 21(1): p. 134-47.
- McPherson, K., C.M. Steel, and J.M. Dixon, ABC of breast diseases. Breast cancer-epidemiology, risk factors, and genetics. BMJ, 2000. 321(7261): p. 624-8.
- Hamajima, N., et al., Alcohol, tobacco and breast cancer–collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer, 2002. 87(11): p. 1234-45.
- Mezzetti, M., et al., Population attributable risk for breast cancer: diet, nutrition, and physical exercise. J Natl Cancer Inst, 1998. 90(5): p. 389-94.
- Boyd, N.F., et al., Mammographic densities and breast cancer risk. Cancer Epidemiol Biomarkers Prev, 1998. 7(12): p. 1133-44.
- Morimoto, L.M., et al., Obesity, body size, and risk of postmenopausal breast cancer: the Women’s Health Initiative (United States). Cancer Causes Control, 2002. 13(8): p. 741-51.
- Friedenreich, C.M., H.K. Neilson, and B.M. Lynch, State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer, 2010. 46(14): p. 2593-604.
- Kahlenborn, C., et al., Oral contraceptive use as a risk factor for premenopausal breast cancer: a meta-analysis. Mayo Clin Proc, 2006. 81(10): p. 1290-302.
- Andrieu, N., et al., Effect of chest X-rays on the risk of breast cancer among BRCA1/2 mutation carriers in the international BRCA1/2 carrier cohort study: a report from the EMBRACE, GENEPSO, GEO-HEBON, and IBCCS Collaborators’ Group. J Clin Oncol, 2006. 24(21): p. 3361-6.
- DeSantis, C.E., et al., Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin, 2014. 64(4): p. 252-71.
- Prosnitz, L.R. and I.S. Goldenberg, Radiation therapy as primary treatment for early stage carcinoma of the breast. Cancer, 1975. 35(6): p. 1587-96.
- Weber, E. and S. Hellman, Radiation as primary treatment for local control of breast carcinoma. A progress report. JAMA, 1975. 234(6): p. 608-11.
- Mock, V., et al., Effects of exercise on fatigue, physical functioning, and emotional distress during radiation therapy for breast cancer. Oncol Nurs Forum, 1997. 24(6): p. 991-1000.
- Payne, D.K., M.D. Sullivan, and M.J. Massie, Women’s psychological reactions to breast cancer. Semin Oncol, 1996. 23(1 Suppl 2): p. 89-97.
- Spiegel, D., Psychosocial aspects of breast cancer treatment. Semin Oncol, 1997. 24(1 Suppl 1): p. S1-36-S1-47.
- Spiegel, D., J.R. Bloom, and I. Yalom, Group support for patients with metastatic cancer. A randomized outcome study. Arch Gen Psychiatry, 1981. 38(5): p. 527-33.
- Kissane, D.W., et al., Cognitive-existential group psychotherapy for women with primary breast cancer: a randomised controlled trial. Psychooncology, 2003. 12(6): p. 532-46.
- Kissane, D.W., et al., Effect of cognitive-existential group therapy on survival in early-stage breast cancer. J Clin Oncol, 2004. 22(21): p. 4255-60. http://thescrutinizer.net/wp-content/uploads/2015/04/Breast-Cancer-CarolYu.jpg
Its excellent as your other blog posts : D, thanks for putting up. “Say not, ‘I have found the truth,’ but rather, ‘I have found a truth.'” by Kahlil Gibran.