By Suchitra Chari, M.S.
 Blood Pressure (BP) is the force per unit area exerted by the circulating blood on the walls of the arteries or blood vessels. Hence, the heart is the organ that generates the pressure and the arteries are the ones that receive the pressure.
Blood Pressure (BP) is the force per unit area exerted by the circulating blood on the walls of the arteries or blood vessels. Hence, the heart is the organ that generates the pressure and the arteries are the ones that receive the pressure.
When we hear the word blood pressure (BP), there are two numbers that come to the mind. One is the top number or the systolic number (Systolic Blood Pressure or SBP). This measures the pressure in the arteries when the heart muscle contracts or beats. The other is the bottom number or the diastolic number (Diastolic Blood Pressure or DBP) that measures the pressure in the arteries when the heart muscle is resting or when it is between the beats. Hypertension (HBP) is a condition in which the either one of the numbers is higher than the normal level.
How is BP measured?
Blood Pressure is measured using an instrument called the sphygmomanometer 1. The unit of measurement of BP is millimeters of mercury (mm Hg). The device comprises of an inflatable cuff, a measuring unit (the mercury manometer or aneroid gauge) and a means to inflate the cuff (usually a manually operated bulb and valve or a pump operated electrically). The manual sphygmomanometers are used in conjunction with a stethoscope. The cuff is placed around the upper arm and is inflated using the bulb. This restricts the blood flow and the blood pressure increases. The cuff is then released to release the pressure while continuously noting the mercury in the column. This release of pressure makes the blood flow through the arteries again and we hear a pounding sound. The point where the sound is first heard is the SBP and is the peak pressure in the arteries during the cardiac cycle. The cuff is further released slowly. The point where the pounding sound stops is the DBP. This is the lowest pressure at the resting phase of the cardiac cycle.
What is the current recommended readings for blood pressure?
This chart reflects blood pressure categories in adults (measured in millimetres of mercury or mm Hg) as defined by The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure 2:
|
Blood Pressure |
Systolic |
Diastolic |
JN7 Category |
|
|---|---|---|---|---|
|
Optimal |
< 120 |
and |
< 80 | Normal |
|
Normal Borderline |
120 – 129 |
or |
80 – 84 |
Prehypertension |
|
Hypertension |
> 140 180 | or | > 90 |
Hypertension |
|
Stage 1 Stage 2 Stage 3 or Hypertensive Crisis |
140 – 159 160 – 179 > 180 180 |
or or or |
90 – 99 100 – 109 > 110 |
Stage 1 Stage 2 Stage 2 |
Let’s start explaining what the terms mean. When the BP is less than 120/80 mm Hg the person is said to be in the green zone meaning he or she does not have hypertension. Hence, this is considered normal blood pressure. At this level with diet and lifestyle changes the heart remains healthy. A category called Prehypertension exists when the person’s BP is elevated above normal (numbers shown in table) but is not as high as in hypertension. A single high reading does not necessarily mean the person has high blood pressure. So, when the readings are above normal (be it prehypertension or hypertension) the doctor will check the person’s pressure two to three times on at least two separate occasions. This is to account for the variability in the readings due to various conditions. BP can fluctuate at different times of the day, in clinical settings when a person is anxious (this is a condition known as white-coat hypertension) and depending on which arm the measurement is taken. If the measured pressure reads 140/90 or above (systolic 140 or above OR diastolic 90 or above) the person is supposed to have Stage 1 Hypertension. Stage 2 Hypertension occurs when the SBP is 160 or above and/or the DBP is 100 or above. For both stage 1 and stage 2 HBP a treatment program is usually initiated immediately along with prescription drugs and lifestyle changes. A systolic reading of 180 mm Hg or higher OR a diastolic reading of 110 mm Hg or higher will need emergency care right away as we then have a condition known as hypertensive crisis.
Both numbers are equally important but generally as a person gets older (50 and above) more emphasis is given to the top number due to a number of factors (stiffness of large arteries, build-up of plaque etc.). A condition called isolated systolic hypertension could occur at this age where the diastolic pressure is normal but systolic pressure is high. Under 50 years, the DBP is more important.
Signs and Symptoms of HBP:
Symptoms are practically absent for people with mild to moderate blood pressure. Even if symptoms like dull headaches, dizzy spells or a few more nosebleeds than usual occur it is easy to mistake these for any other condition. Hence starting at age 18, it is best to check your pressure at least once every 2 years.
Once detected with HBP, routine tests such as a urine test (urinalysis), blood tests, an electrocardiogram (a test that measures the heart’s electrical activity) and sometimes a cholesterol test are recommended by the doctor. An important step once you are detected with HBP is to measure your BP at home. This will keep your blood pressure in check and ensure that the treatment works.
Now, why should we be worried about hypertension? To know this, we need to know a little bit about the heart and its functioning.
The Heart:
Circulating blood in the body has to be constantly purified. This is done with the help of the lungs using the oxygen rich-air we breathe in. Thus blood in the heart goes to the lungs to get oxygenated and re enters the heart. There are a total of 4 chambers in the heart; two auricles or atria on the top and two ventricles in the bottom. The ventricles contract to pump this oxygenated blood to the rest of the body through blood vessels called arteries. This blood is needed by the organs to carry out their daily functions. When the ventricles contract (when the heart is beating), the blood is pushed through the arteries with a certain amount of force or tension. The force of the blood running through the arteries causes a pressure on the walls of the arteries. Arteries or blood vessels are of two kinds. One is the medium to large arteries (thickness ranging from 25 mm to 1mm) and the other is the smaller arteries and arterioles that are present in organs (thickness ranging from 1 mm to 0.01 mm)
During this cardiac cycle of the heart the maximum pressure exerted during the contraction of the ventricles is the SBP and the minimum pressure exerted during the relaxation of the ventricles is the DBP. This, as we said earlier is 120 / 80 mm Hg under normal conditions. During hypertension, there is something that causes tension or more pressure on the walls of the arteries and thus the blood pressure rises. Now let us look into how this rise in readings occurs.
Blood Pressure Equation:
In scientific terms, blood pressure or the mean arterial pressure is defined as a combination of cardiac output (CO) and Peripheral Resistance (PR) or Systemic Vascular Resistance. CO is the amount of blood each ventricle of the heart is pumping out per minute and PR is the amount of resistance to blood flow in the arteries.
So the equation goes like this:
Blood Pressure = Cardiac Output x Peripheral Resistance.
Now CO can be calculated the following way:
CO = Heart Rate x Stroke Volume
Where Heart Rate (HR) is the number of beats per minute and Stroke Volume (SV) is the amount of blood each ventricle is pumping with each circulation.
Hence Blood Pressure will increase when either CO or PR is increased.
Pathogenesis of HBP:
The pathogenesis of HBP involves 5 organs in the body: the heart, the brain and spinal cord, the adrenal glands (endocrine glands that produce a lot of hormones), the blood vessels and the kidneys. We need to know the role played by each of these to understand how the drugs work in our body. There are 2 systems that play a major role in BP. One is the Renin-Angiotensin-Aldosterone Pathway and the other is the Sympathetic Nervous System (SNS). We will discuss these below.
Renin-Angiotensin-Aldosterone System3:
Due to stress or increased work load, sympathetic nervous system activity (the one that controls the fight, fright and flight hormone) is activated. This causes the smooth muscles around the blood vessels to contract which causes the narrowing of the arteries causing more resistance to blood flow. Hence PR increases. This is known as Increased Artireolar Vasoconstriction. The BP thus increases. One of the vital organs that gets affected due to this increased PR is the kidney. Blood flow thus decreases to the kidneys. When blood flow to the kidney is decreased (low renal perfusion), the production of an enzyme called renin is stimulated in the kidneys. This starts a chain of chemical steps.
1.Angiotensinogen is an inactive prohormone that is produced in the liver and released into the blood. The rennin produced in the kidneys converts angiotensinogen to Angiotensin 1 (Ang 1). Angiotensin is a chemical that causes the arteries to become narrow or constrict, especially in the kidneys but also throughout the body. Then an enzyme called Angiotensin Converting Enzyme (ACE) converts Ang 1 to Angiotensin 2 (Ang 2).
Ang 2 has a number of effects:
# It causes systemic vasoconstriction in the arteries. This leads to increased BP due to increased PR.
# It causes increased sodium reabsorption in the kidney tubules; hence also causes increased water reabsorption. The fluid balance maintained by the kidney gets offset and blood volume (BV) increases. When the BV increases, the heart pumps out more blood outside when it contracts thus increasing CO.
# It stimulates the conversion of steroid precursors in the adrenal glands to a steroid hormone, Aldosterone. This hormone also causes increased sodium and water reabsorption .
The combination of vasoconstriction and sodium reabsorption causes an increase in BP. This BP causes more damage to the walls of the arteries which in turn causes less Blood Flow and the whole cycle continues again.
Sympathetic Nervous System (SNS) (A part of the Autonomous Nervous System):
When decreased systemic blood pressure occurs (controlled by the negative feedback system, the baroreceptors present at the corotid sinus and aortic arch) signals are sent to the brain stem through cranial nerves. At this point the SNS of the Autonomic nervous system sends new signals via the spinal cord to different tissues.
# Some signals travel through peripheral nerves that releases a hormone called norepinephrine. This hormone is released locally in 2 locations. One is in the heart where it increases heart rate and myocardial contractility through beta 1 receptors and the second is in the blood vessel where it causes systemic vasoconstriction through alpha 1 receptors.
# Some signals act in the adrenal glands to release systemic epinephrine and some systemic norepinephrine both of which travel through the bloodstream and reinforce the action of the local Norepinephrine in the heart and blood vessels.
Types of Hypertension:
Primary or Essential Hypertension:
This kind of hypertension develops slowly over years. Essential hypertension4 is usually associated with a reading of 140 / 90 mm Hg or above. It is asymptomatic (does not show any signs or symptoms) and may not be detected unless regular check-ups are done. Essential hypertension accounts for greater than 95% of all cases of hypertension. This kind of HBP occurs due to indirect causes. Among them,tThe modifiable factors are obesity, smoking, sedentary lifestyle, excess salt intake and excess alcohol. The non-modifiable ones are family history, age (risk of getting HBP greater after 50 years) and race (African Americans are more prone to get HBP). Stress is also considered a major risk factor.
Secondary Hypertension:
This usually has a direct or an identifiable cause5 and has a high value. Less than 5% of people with HBP fall in this category.
The more common conditions that could lead up to this hypertension are kidney dysfunction (renovascular disease, renal failure), renovascular hypertension (narrowing of one or both of the arteries leading to the kidneys), hyperaldosteroidism, pregnancy-induced hypertension or preeclampsia and certain medications and supplements (birth control pills, cold remedies, decongestants, and over-the-counter pain relievers, illegal drugs like cocaine and amphetamines).
The less common reasons are diabetes complications like diabetic nephropathy, thyroid problems, certain congenital defects like coarctation or a narrowing of the aorta, pheochromocytoma (a rare tumour in the adrenal gland), aldosteronism (again a tumour in the adrenal gland), cushing syndrome (excess production of a steroid hormone called cortisol in the adrenal glands) and obstructive sleep apnea.
HBP can also occur in children if they already have an existing problem in their kidney or heart6. Recently kids who have poor lifestyle habits, such as an unhealthy diet, obesity and lack of exercise are susceptible to HBP at a young age.
Resistant hypertension: When your blood pressure is difficult to control:
A blood pressure that is resistant to treatment is known as resistant hypertension7. In this case the HBP remains high despite taking at least three different types of high blood pressure drugs, where one is a diuretic. At this point once the cause has been identified, there’s a good chance you can meet your goal with the help of treatment that’s more effective. Medications have to be fine-tuned to come up with the most effective combination and doses. Also, medications taken for other conditions have to be reviewed.
If the high blood pressure medications are not taken exactly as directed (reasons being not being able to afford the medication, side effects or simply forgetting), your blood pressure can pay the price. Talking to the doctor about the problems is a better way to solve the rather than resorting to solutions on our own. Also the treatment should not be changed without the doctor’s guidance as each person’s body is unique and drugs are prescribed according to an individual’s case.
Hypertensive Crisis:
This HBP occurs when there is a systolic reading of 180 mm Hg or higher OR a diastolic reading of 110 mm Hg8.
It has 3 categories.
# Severe HBP plus no symptoms and no acute end organ dysfunction is known as hypertensive urgency. This is not life-threatening and can be treated in an outpatient facility.
# Severe HBP plus symptoms and/or acute end organ dysfunctions is known as hypertensive emergency.
# Severe HBP plus retinal haemorrhages and/or pappiledema (optic disc swelling that is caused by increased intracranial pressure) is known as malignant hypertension.
The last 2 conditions are life threatening and the patient needs to be admitted to get treated.
When should a person with primary hypertension be screened for secondary hypertension?
# When they have resistant hypertension
# When they have a hypertensive emergency
# When they get HBP at less than 30 years without having any risk factors
# When they get HBP before puberty irrespective of risk factors
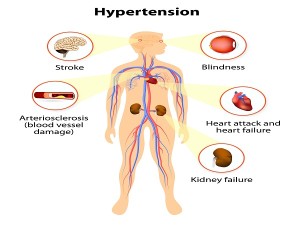
What are the complications due to hypertension?
As mentioned earlier, most people having primary HBP do not show any symptoms initially till it crosses a certain point. In such cases, if untreated, HBP can cause complications. How do these complications occur due to HBP?
# Due to the pressure exerted on the arteriolar walls, hypertension can cause hardening and thickening of the arteries and make them very firm. This causes a condition called arteriosclerosis. This condition can lead to coronary heart disease, a heart attack or a stroke.
# Increased blood pressure can cause a part of the blood vessel to be weakened and bulge changing the shape of its wall. This damage could get bigger and ultimately give way bursting the blood vessel. This is a haemorrhage or aneurysm. This is life threatening. In the case of smaller arteries that are present in organs, this haemorrhage could lead to organ damage like kidney failure and retinopathy or loss of vision.
# The heart muscle thickens over time as it has to work harder to pump blood due to the high pressure. This thickened muscle will then have an even tougher time pumping enough blood to meet the body’s needs leading to a heart failure.
# Metabolic syndrome is a cluster of syndromes of which HBP is one of them. The others are diabetes, excess body fat around the waist and abnormal cholesterol levels. The more components you have, the greater the risk of developing heart disease, diabetes or stroke.
# Uncontrolled blood pressure can lead to having problems with memory or understanding
# Peripheral vascular diseases (PVDs) are circulation disorders that affect blood vessels outside of the heart and brain. In PVD, the blood vessels are narrowed usually caused by arteriosclerosis. HBP is one of the risk factors for PVD.
Treatment and Drugs:
Below are the new guidelines for treatment of high blood pressure in adults according to an article by Jill Jin, MD, MPH in JAMA published in 2014,
# For a person younger than 60 years: When the systolic is 140 mm Hg or higher and/or the diastolic is 90 mm Hg or higher.
# For a person 60 years or older: When the systolic is 150 mm Hg or higher and/or the diastolic is 90 mm Hg or higher.
# For a person with chronic kidney disease or diabetes at any age: When the systolic is 140 mm Hg or higher and/or when the diastolic is 90 mm Hg or higher
Medications:
Two major criteria decide which mediation to use:
1.Underlying diagnosis of the patient
2.Comorbidities (any additional disease the patient might have)
Treatment with pharmacological agents (drugs)
To reduce the number of daily medication doses one needs, the doctor may prescribe a combination of low-dose medications rather than larger doses of one single drug. In fact, two or more blood pressure drugs may be more effective than one. Sometimes finding the most effective medication or combination of drugs is a matter of trial and error.
We can divide medications into 2 major categories depending on which pathway they work in.
1.Drugs that act on the Renin-Angiotensin-Aldosterone Pathway:
Renin Inhibitors ACE Inhibitors ARBs
↓ ↓ ↓ 1. Systemic Vasoconstriction
Angiotensinogen——Renin—–Ang 1——–ACE———Ang 2—————-2. Renal sodium reabsorption ← Diuretics
3. Production of Aldosterone————– Renal sodium reabsorption ← Diuretics
↑
Aldosterone Inhibitors
ACE (Angiotensin Converting Enzyme) inhibitors:
# ACE inhibitors block the enzyme ACE thus preventing the conversion of Ang 1 to Ang 2
# They thus help the body produce less angiotensin. This helps the blood vessels relax and open up, which, in turn, lowers blood pressure.
# They are most effective in young white population, people with chronic kidney disease, patients with diabetes as it protects their kidneys
# Benefits are improving ejection fraction (EF) in patients with Congestive Heart Failure (CHF) thus improving survival; also improves survival in post Myocardial Infarction (MI) or Heart Attack
Diuretics:
# Diuretics are a broad category of drugs that include thiazide diuretics, loop diuretics and potassium sparing diuretics
# Act on the kidneys and help the body get rid of excess sodium (salt) and water. This reduces blood volume and helps control blood pressure9. They are often used in combination with additional prescription therapies.
# They are often the first10, but not the only, choice in high blood pressure medications
# They are most effective in African American people and in the elderly11
Angiotensin II receptor blockers (ARBs):
# ARBs block the action of Ang 2 by blocking its attachment to its receptor.
# Thus the blood vessel is not constricted but stays open and blood pressure is reduced.
# They are most effective in young white population, people with chronic kidney disease, patients with diabetes as it protects their kidneys
# Benefits are improving ejection fraction (EF) in patients with Congestive Heart Failure (CHF) thus improving survival; also improves survival in post Myocardial Infarction (MI) or Heart Attack
# Side effects are angioedema where the tongue swells, cough and increase in Na, K and Creatine
Aldosterone antagonists: These drugs block the effect of aldosterone thus reducing salt and fluid retention
Renin Inhibitors: These inhibit the action of rennin thus preventing the formation of angiotensin
2. Drugs that act on the Sympathetic Nervous System
Beta Blockers Calcium Channel Blockers (Dihydropyridines or DHP)
↓ ↓
—–1. Local Norepinephrine in the heart——————–beta 1 receptors——-Increased heart rate and myocardial contractility
Centrally acting alpha 2 agonists Beta and Alpha Blockers
↓ ↓
Decreased Systemic BP—–Brain——SNS —–2. Systemic epinephrine and systemic norepinephrine——————–reinforce activity of norepinephrine in heart and blood vessel
Alpha Blockers1
—–3. Local norepinephrine in the blood vessels—————alpha 1 receptors——Systemic Vasoconstriction
↑
Calcium Channel Blockers (Non-Dihydropyridines or Non-DHP)
Beta Blockers:
# These block epinephrine and norepinephrine activities at beta adrenergic receptors.
# Thus they reduce the heart rate, which reduces the heart’s workload thus opening up the blood vessels which then increases the heart’s output of blood, causing the heart to beat slower and with less force. This lowers blood pressure.
# Not recommended as the only choice of drug nowadays12
# Most effective in young white population
# Benefits include it improves survival in patients with CHF and in post Myocardial Infarction (MI) or Heart Attack
# don’t work as well, especially in older adults, but may be effective when combined with other blood pressure medications
Alpha blockers:
# These block epinephrine and norepinephrine activities at alpha adrenergic receptors.
# They reduce systemic vasoconstriction
Calcium Channel Blockers:
# There are 2 sub group. The Dihydropyridines (DHP) inhibit the systemic vasoconstriction. The non-dihydropyridines (non-DHP) inhibit the heart rate and contractility.
# Act by relaxing the muscles of your blood vessels. Some slow your heart rate
# Mechanism of action is by preventing calcium from entering the smooth muscle cells of the heart and arteries13. The effect of contraction of the heart muscles by calcium is reduced. Calcium channel blockers thus relax and open up narrowed blood vessels, reduce heart rate and lower blood pressure.
# They are most effective In African American people and in the elderly
Central-acting alpha 2 agonists:
# Act directly on the brain and decrease the activity of the sympathetic nervous system thus increasing heart rate and narrow your blood vessels. They help decrease the blood vessels’ ability to tense up or contract. Although, they follow a different nerve pathway than the alpha and beta-blockers, they accomplish the same goal of blood pressure reduction. Methydopa is an example of this category and is the first line of therapy during pregnancy due to decreased side effects for both the mother and the foetus.
Most of the bottom table is taken from a Youtube lecture by Eric, a Professor at Stanford University.
[custom_table]| Drug Class | Common Suffix | Common examples | Important Side Effects |
|---|---|---|---|
| ACE Inhibitors | -pril | Lisinopril, Enalopril, Benazepril, Fosinopril | Dry cough, renal dysfunction (increase in Na+, K+ and creatine), angioedema |
| Thiazide Diuretics | None | Hydrochlorothiazide, Chlorthiazide, Chlorthalidone | ↓ Na+ and K+ in the blood, renal dysfunction, ↑ insulin resistance – hence not recommended for diabetes patients |
| Loop Diuretics | None | Furosemide, Bumetanide, Torsemide | ↓ Na+ and K+ in the blood, renal dysfunction |
| DHP Calcium Channel Bockers | -dipine | Amlodipine, Felodipine, Nicardipine, Nifedipine | Constipation, lower extremity edema, ↑ heart rate (except for Amlodipne) |
| Non-DHP Calcium Channel Blockers | None | Diltiazem, Verapamil | ↓ Myocardial Contractility, ↓ heart rate |
| ARBs | -sartan | Losartan, Valsartan, Irbesartan | Renal Dysfunction |
| Beta Blockers | -olol | Metoprolol, Carvedilol, Labetalol, Propranolol, Esmolol | ↓ Myocardial Contractility (acutely), ↓ heart rate, fatigue, sexual dysfunction, depression, ↑ lipids, cholesterol, asthma and bronchiospasm |
| Alpha Blockers | -osin | Terazosin, Prazosin, Doxazosin | Orthostatic Hypotension (sudden drop in BP when standing up) |
Other Drugs that do not act through the above systems:
Nitrates act by inducing venodilation. Venodilation reduces blood return to the heart. This decreases cardiac output.
Vasodilators. These medications work directly on the muscles in the walls of your arteries, preventing the muscles from tightening and your arteries from narrowing. This allows blood to flow through better.
Peripheral adrenergic inhibitors: Prevents the release of norepipephrine at nerve endings and hencehis blocks the smooth muscles from getting the “message” to constrict.
Lifestyle changes (non-pharmocologicxal modifications) are as important as medications with regards to HBP. Owing to the high side effects of hypertensive medications, lifestyle changes are beneficial as they can help us reduce the dose. The most important of these changes are:
# Low sodium diet: To consider here is the DASH (Dietary Approaches to STOP Hypertension) diet rich in nuts, whole grains, fruits, vegetables and low-fat dairy foods. A sodium level of 1500 milligrams a day is ideal for people 51 years of age and older. Avoiding processed foods will keep the sodium in check.
# Aerobic exercise: At least 30 minutes of physical activity a day like jogging, cycling, swimming and even mild weight lifting will help lower blood pressure.
# Maintenance of a healthy weight: Weight reduction of at least 10-30 lbs helps a lot in reducing BP
# Quitting smoking: Tobacco injures blood vessel walls and thus speeds up the process of hardening the arteries
# Limiting alcohol: One drink a day and not more than that for healthy adults is a good amount
# Reducing stress: Practising relaxation or slow, deep breathing. Getting plenty of sleep also helps.
# Monitoring blood pressure at home: This helps keep close tabs on it, to show if medication is working, and even alert you and your doctor to potential complications
Coping with hypertension can be hard especially since it is a condition that we need to manage for the rest of our lives. But with lifestyle changes, good support from family and periodical doctor visits one can easily manage this disease and live healthy for a long time without any complications.
References:
1. Jeremy Booth. A Short History of Blood Pressure Measurement. Section of the History of Medicine Paper Volume 70 November 1977
2. Chobanian AV, Bakris GL, Black HR et al. (December 2003). “Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure”. Hypertension 42 (6): 1206–52 CS1 maint: Explicit use of et al. (link)
3. Paul M, Poyan Mehr A, Kreutz R (July 2006). “Physiology of local renin-angiotensin systems”. Physiol. Rev. 86 (3): 747–803
4. Carretero OA, Oparil S (January 2000). “Essential hypertension. Part I: definition and etiology”. Circulation 101 (3): 329–35
5. ANTHONY J. VIERA and DANA M. NEUTZE. Diagnosis of Secondary Hypertension: An Age-Based Approach
FREE PREVIEW. AAFP members and paid subscribers: Log in to get free access. All others: Purchase online access.
FREE PREVIEW. Purchase online access to read the full version of this article. Am Fam Physician. 2010 Dec 15;82(12):1471-1478
6. Flynn JT. Evaluation and management of hypertension in childhood. Prog Pediatr Cardiol. 2001;12(2):177-188
7. Calhoun DA, Jones D, Textor S et al. (June 2008). “Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research”. Hypertension 51 (6): 1403–19
8. Rodriguez MA1, Kumar SK, De Caro M. Hypertensive crisis. Cardiol Rev. 2010 Mar-Apr;18(2):102-7
9. Julio D Duarte1 and Rhonda M Cooper-DeHoff. Mechanisms for blood pressure lowering and metabolic effects of thiazide and thiazide-like diuretics Expert Rev Cardiovasc Ther. 2010 June ; 8(6): 793–802.
See comment in PubMed Commons below10 Fuchs FD. Diuretics: drugs of choice for the initial management of patients with hypertension. Expert Rev Cardiovasc Ther. 2003 May;1(1):35-41
11. Morgan TO, Anderson AI, MacInnis RJ. ACE inhibitors, beta-blockers, calcium blockers, and diuretics for the control of systolic hypertension Am J Hypertens. 2001 Mar;14(3):241-7
12.Beevers DG. The end of beta-blockers for uncomplicated hypertension? Lancet. 2005; 366:1510-1512
13.Godfraind, T. & Kaba, A. (1969a) Blockade or reversal of the contraction induced by calcium and adrenaline in depolarized arterial smooth muscle. Br. J. Pharmacol. 36, 549–560