By Catherine Murari-Kanti, M.S.
 Introduction:
Introduction:
Folic acid received its name from the Latin word folium which means leaf since it was isolated from spinach leaves in 1941. [1] Folic acid is also called Vitamin B9 making it part of the B-complex of vitamins and folate is the active form that is found in food and in the human body required for its functions. Folic acid has no biological activity unless its converted into the active form of folate. [2]
Conversion to active form
Figure adapted from [3]
When folic acid enters your system from your diet, it usually has to convert to the folate form for efficient use. Food folates like polyglutamates and monoglutamates (parent compounds) get converted in the gut to dihydrofolate (DHF) and tetrahydrofolate (THF) respectively which is then converted to 5-methyl tetrahydrofolate with the help of the enzyme 5,10 methylenetetrahydrofolate reductase (MTHFR). 5-methyl THF is the active form of folic acid found in the plasma. [3]
Structure of Folic acid:
Molecular Formula: C19H19N7O6 [4]
Functions:
- Folates mediate the transfer of one-carbon units in various reactions that are critical to nucleic acid (DNA and RNA) and amino acid (building blocks of proteins) synthesis and metabolism. Folates are involved in the conversion of homocysteine to methionine in the synthesis of S-adenosyldeoxyuridylate (SAM) which acts as methyl donor as well as in methylation of deoxyuridylate to thymidylate to form DNA. [5, 6]
- Folic acid, Vitamin B12 regulate the concentration and metabolism of homocysteine (an intermediate in the synthesis of sulfur-containing amino acids)[7]
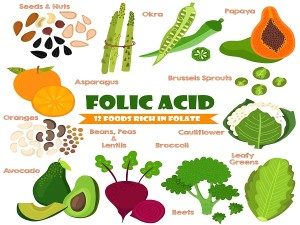
Dietary sources of Folic acid:[2, 8]
- Dark green leafy vegetables (Spinach, Swiss chard, Broccoli, Arugula, Collard greens and Dandelion greens) can be incorporated in salads and eaten raw for maximal effect.
- Dried beans and peas (legumes)
- Dairy products, poultry, meat, eggs and seafood
- Citrus fruits and juices
- Fortified cereal, flours, breads, pastas, rice and other grain products [9]
Dietary requirements:
The Food and Nutrition Board of the US Institute of Medicine coined a new term called “Dietary Folate Equivalent (DFE)” which reflects the higher bioavailability of folic acid than that of food folate. [2, 10]
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| 0-6 months | 65 mcg* DFE | 65 mcg* DFE | ||
| 7-12months | 80 mcg* DFE | 80 mcg* DFE | ||
| 1-3 years | 150 mcg DFE | 150 mcg DFE | ||
| 4-8 years | 200 mcg DFE | 200 mcg DFE | ||
| 9-13 years | 300 mcg DFE | 300 mcg DFE | ||
| 14-18 years | 400 mcg DFE | 400 mcg DFE | 600 mcg DFE | 500 mcg DFE |
| 19+ years | 400 mcg DFE | 400 mcg DFE | 600 mcg DFE | 500 mcg DFE |
*0-12 month infants get the required amount of folate from breast milk
Individuals at risk for folate deficiency:
- Alcohol dependent individuals because of a poor diet associated with their lifestyle. Alcohol consumption of even 8 fluid ounces a day for 2 weeks can cause a significant decrease in serum folate concentrations. [11]
- Women of childbearing age require plenty of folate because its deficiency is responsible for varied birth defects. Pregnant women are more likely to have folate deficiency because of the increased need of folate for RNA and DNA synthesis. 600mcg/day is what a pregnant woman should be taking and it could be hard to get that amount from diet alone and therefore a prenatal vitamin would be a good supplement of choice. [12, 13]
- Individuals with malabsorptive disorders like celiac disease, inflammatory bowel disease and tropical spruce may not be able to fully absorb folate like people without these disorders. [14]
Deficiency of folate:
Folate deficiency causes megaloblastic anemia. Blood cells are produced in the bone marrow and since rapidly growing and dividing cells require folate for DNA and RNA needs, in the presence of inadequate folate blood cells would look immature, enlarged and fewer in number. Normal blood cells have 4 month life span and therefore there is usually a 4 month lag period before the symptoms of megaloblastic anemia are observed. Some of these symptoms include shortness of breath, fatigue, weankness, difficulty concentrating, headaches and heart palpitations. [2] Megaloblastic anemia caused by folate deficiency is similar to the one caused by Vitamin B12 deficiency and more tests should be conducted to confirm the source of the anemia. Intake of folic acid should be able to reverse the symptoms and deficiency is extremely rare in the United States since most of our foods are fortified. [15]
Folate deficiency in pregnancy:
- Neural tube defects: DNA and RNA synthesis are the hallmarks of new life progression after conception for which folate is extremely necessary. The neural tube is responsible for the proper development of the nervous system which occurs 21-28 days after conception when the mother is usually unaware of her pregnancy. In the presence of inadequate folate conditions like exencephaly (brain grows outside the skull), anencephaly (parts of the brain and skull are missing) and spinabifida (incomplete closure of the neural tube) could occur which are life threatening. [16, 17]
- Cardiovascular defects: Congenital cardiovascular defects cause high number of infant death and responsible for poor heart health in adults. Studies have shown that mothers who took atleast 400 mcg folate daily reduced the risk of congenital cardiovascular disease by 18%. [18, 19]
- Orofacial defects: Another congenital deformity is the cleft lip with or without cleft palate which in a study, showed a decrease with an intake of folic acid along with a multivitamin. [20, 21]
Toxicity:
Folic acid is a water soluble vitamin, easily excreted by the body and therefore has minimal risk of toxicity. However if folic acid is taken in huge amounts to correct megaloblastic anemia then it could mask the neurological effects of Vitamin B12 which also causes megaloblastic anemia. Therefore it is very necessary to figure out the source of megaloblastic anemia and be treated accordingly. [2]
High supplementation of folic acid has been recently associated with progression of preneoplastic lesions and therefore increasing the risk of colorectal cancer. [22–24]
Folate and health:
Cancer:
The consensus on cancer and folate is mixed. Obviously folic acid would influence the development of cancer because of its role as a one-carbon donor and thus its effect on DNA synthesis and cell replication. [25, 26] One study suggests that there was no effect of folic supplementation on cancer outcomes while the other showed that there was an increase in cancer incidence with folic acid supplementation. [27, 28]
Most work in figuring out the relationship between cancer and folate supplementation has been done in colorectal cancer. These studies have shown an inverse relationship between folate supplementation and colorectal adenoma or carcinoma risk. [29–31] However, there are other studies where folic acid supplementation didn’t increase or decrease the risk of colorectal adenoma or carcinoma. [32, 33] More research needs to be done to understand the relationship between folic acid and cancer.
Cardiovascular diseases/Stroke:
Folate and other B vitamins are associated with the regulation and metabolism of homocysteine and they can reduce the risk of cardiovascular disease and stroke by lowering homocysteine levels. [2, 34] There is a higher possibility of lowering the risk of stroke than cardiovascular disease. [34–40]
Interactions with some medications:
| Drug | Interaction with Folic acid |
|---|---|
| Methotrexate | Folate antagonist (folic supplements will interfere with cancer treatment) [41] |
| Antiepileptic medications | Reduce serum levels of folate (folic supplements will reduce serum levels of drugs) [42] |
| Sulfasalazine (for ulcerative colitis) | Inhibits folate absorption – causes folate deficiency [43] |
| Antibiotics & Tetracyclines | Folic acid prevents the absorption of the drugs |
| Chemotherapy drugs | Talk to your doctor before taking |
| Pyrimethamine (Anti-malaria) | Folic acid reduces effectiveness of drug |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Lowers folic acid levels |
Note: All vitamins are good for health and should be taken with moderation. Make sure you speak to your doctor before adding any supplement to your routine to make sure it doesn’t interfere with any other medication you may be taking.
References:
1. Mitchell, H.K., E.E. Snell, and R.J. Williams, Journal of the American Chemical Society, Vol. 63, 1941: The concentration of “folic acid” by Herschel K. Mitchell, Esmond E. Snell, and Roger J. Williams. Nutr Rev, 1988. 46(9): p. 324-5.
2. Institute of, M., Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. 1998, Washington, DC: The National Academies Press. 592.
3. Pietrzik, K., L. Bailey, and B. Shane, Folic Acid and L-5-Methyltetrahydrofolate. Clinical Pharmacokinetics. 49(8): p. 535-548.
4. Hamed, E., M.S. Attia, and K. Bassiouny, Synthesis, spectroscopic and thermal characterization of copper(II) and iron(III) complexes of folic acid and their absorption efficiency in the blood. Bioinorg Chem Appl, 2009: p. 979680.
5. Bailey, L.B. and J.F. Gregory, 3rd, Folate metabolism and requirements. J Nutr, 1999. 129(4): p. 779-82.
6. Jacques, P.F., et al., The relationship between riboflavin and plasma total homocysteine in the Framingham Offspring cohort is influenced by folate status and the C677T transition in the methylenetetrahydrofolate reductase gene. J Nutr, 2002. 132(2): p. 283-8.
7. Gerhard, G.T. and P.B. Duell, Homocysteine and atherosclerosis. Curr Opin Lipidol, 1999. 10(5): p. 417-28.
8. United States Department of Agriculture Agricultural Research Service National Nutrient Database for Standard Reference Release 27 [cited 2015 April 30]; Available from: http://www.ars.usda.gov/sp2UserFiles/Place/80400525/Data/SR27/sr27_doc.pdf.
9. Dietrich, M., C.J. Brown, and G. Block, The effect of folate fortification of cereal-grain products on blood folate status, dietary folate intake, and dietary folate sources among adult non-supplement users in the United States. J Am Coll Nutr, 2005. 24(4): p. 266-74.
10. Institute of Medicine, Food and Nutrition Board 1998 [cited 2015 May 1]; Available from: http://www.iom.edu/~/media/Files/Activity%20Files/Nutrition/DRIs/New%20Material/2_%20RDA%20and%20AI%20Values_Vitamin%20and%20Elements.pdf.
11. Gloria, L., et al., Nutritional deficiencies in chronic alcoholics: relation to dietary intake and alcohol consumption. Am J Gastroenterol, 1997. 92(3): p. 485-9.
12. Scholl, T.O. and W.G. Johnson, Folic acid: influence on the outcome of pregnancy. Am J Clin Nutr, 2000. 71(5 Suppl): p. 1295S-303S.
13. Scholl, T.O., et al., Use of multivitamin/mineral prenatal supplements: influence on the outcome of pregnancy. Am J Epidemiol, 1997. 146(2): p. 134-41.
14. Nutrition and IBD. 2012 [cited 2015 May 1]; Available from: http://www.ccfa.org/resources/nutrition-and-ibd.html.
15. Aslinia, F., J.J. Mazza, and S.H. Yale, Megaloblastic anemia and other causes of macrocytosis. Clin Med Res, 2006. 4(3): p. 236-41.
16. Czeizel, A.E., et al., Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients. 5(11): p. 4760-75.
17. Eskes, T.K., Open or closed? A world of difference: a history of homocysteine research. Nutr Rev, 1998. 56(8): p. 236-44.
18. Gilboa, S.M., et al., Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation. 122(22): p. 2254-63.
19. van Beynum, I.M., et al., Protective effect of periconceptional folic acid supplements on the risk of congenital heart defects: a registry-based case-control study in the northern Netherlands. Eur Heart J. 31(4): p. 464-71.
20. Badovinac, R.L., et al., Folic acid-containing supplement consumption during pregnancy and risk for oral clefts: a meta-analysis. Birth Defects Res A Clin Mol Teratol, 2007. 79(1): p. 8-15.
21. Wilcox, A.J., et al., Folic acid supplements and risk of facial clefts: national population based case-control study. BMJ, 2007. 334(7591): p. 464.
22. Mason, J.B., Unraveling the complex relationship between folate and cancer risk. Biofactors. 37(4): p. 253-60.
23. Kim, Y.I., Folate: a magic bullet or a double edged sword for colorectal cancer prevention? Gut, 2006. 55(10): p. 1387-9.
24. Ulrich, C.M. and J.D. Potter, Folate supplementation: too much of a good thing? Cancer Epidemiol Biomarkers Prev, 2006. 15(2): p. 189-93.
25. Kim, Y.I., Folate and carcinogenesis: evidence, mechanisms, and implications. J Nutr Biochem, 1999. 10(2): p. 66-88.
26. Kim, Y.I., Will mandatory folic acid fortification prevent or promote cancer? Am J Clin Nutr, 2004. 80(5): p. 1123-8.
27. Andreeva, V.A., et al., B vitamin and/or omega-3 fatty acid supplementation and cancer: ancillary findings from the supplementation with folate, vitamins B6 and B12, and/or omega-3 fatty acids (SU.FOL.OM3) randomized trial. Arch Intern Med. 172(7): p. 540-7.
28. Ebbing, M., et al., Cancer incidence and mortality after treatment with folic acid and vitamin B12. JAMA, 2009. 302(19): p. 2119-26.
29. Giovannucci, E., et al., Multivitamin use, folate, and colon cancer in women in the Nurses’ Health Study. Ann Intern Med, 1998. 129(7): p. 517-24.
30. Giovannucci, E., et al., Folate, methionine, and alcohol intake and risk of colorectal adenoma. J Natl Cancer Inst, 1993. 85(11): p. 875-84.
31. Gibson, T.M., et al., Pre- and postfortification intake of folate and risk of colorectal cancer in a large prospective cohort study in the United States. Am J Clin Nutr. 94(4): p. 1053-62.
32. Song, Y., et al., Effect of combined folic acid, vitamin B(6), and vitamin B(12) on colorectal adenoma. J Natl Cancer Inst. 104(20): p. 1562-75.
33. Figueiredo, J.C., et al., Folic acid and prevention of colorectal adenomas: a combined analysis of randomized clinical trials. Int J Cancer. 129(1): p. 192-203.
34. Clarke, R., et al., Effects of lowering homocysteine levels with B vitamins on cardiovascular disease, cancer, and cause-specific mortality: Meta-analysis of 8 randomized trials involving 37 485 individuals. Arch Intern Med. 170(18): p. 1622-31.
35. Huang, T., et al., Meta-analysis of B vitamin supplementation on plasma homocysteine, cardiovascular and all-cause mortality. Clin Nutr. 31(4): p. 448-54.
36. Toole, J.F., et al., Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the Vitamin Intervention for Stroke Prevention (VISP) randomized controlled trial. JAMA, 2004. 291(5): p. 565-75.
37. Lonn, E., et al., Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med, 2006. 354(15): p. 1567-77.
38. Albert, C.M., et al., Effect of folic acid and B vitamins on risk of cardiovascular events and total mortality among women at high risk for cardiovascular disease: a randomized trial. JAMA, 2008. 299(17): p. 2027-36.
39. Ebbing, M., et al., Mortality and cardiovascular events in patients treated with homocysteine-lowering B vitamins after coronary angiography: a randomized controlled trial. JAMA, 2008. 300(7): p. 795-804.
40. Armitage, J.M., et al., Effects of homocysteine-lowering with folic acid plus vitamin B12 vs placebo on mortality and major morbidity in myocardial infarction survivors: a randomized trial. JAMA. 303(24): p. 2486-94.
41. Morgan, S.L. and J.E. Baggott, Folate supplementation during methotrexate therapy for rheumatoid arthritis. Clin Exp Rheumatol. 28(5 Suppl 61): p. S102-9.
42. Linnebank, M., et al., Antiepileptic drugs interact with folate and vitamin B12 serum levels. Ann Neurol. 69(2): p. 352-9.
43. Halsted, C.H., G. Gandhi, and T. Tamura, Sulfasalazine inhibits the absorption of folates in ulcerative colitis. N Engl J Med, 1981. 305(25): p. 1513-7.