By Wendy Brody, Pharm. D.
 Osteoporosis is the most common bone disorder affecting humans12. Bone strength is compromised, thus predisposing one to an increased risk of fractures of the hip, spine and wrists.1Both men and women can develop osteoporosis, although men usually have a lower risk than women.
Osteoporosis is the most common bone disorder affecting humans12. Bone strength is compromised, thus predisposing one to an increased risk of fractures of the hip, spine and wrists.1Both men and women can develop osteoporosis, although men usually have a lower risk than women.
During ones lifetime, old bone is removed (resorption) and new bone is added to the skeleton (formation). During childhood and teenage years, new bone is added faster than old bone is removed, resulting in larger, heavier and denser bones. Bone formation outpaces resorption until peak bone mass (maximum bone density and strength) is reached around age 30.2Beyond that time, bone resorption slowly starts to exceed bone formation. Women have their fastest bone loss in the first few years after menopause, and it continues into the postmenopausal years. Osteoporosis develops when bone resorption occurs too quickly or when replacement occurs too slowly.
However, osteoporosis is not always the result of bone lossas is the case in those individuals who did not reach peak bone mass during their bone building years.12 They may have low bone density without much actual bone loss. Figure 1 shows a microscopic view comparing what osteoporotic bone matrix looks like compared to normal bone matrix. It is easy to see the fragility of the osteoporotic bone compared to the normal bone.
Osteoporosis is categorized as either primary or secondary. Primary osteoporosis is usually due to bone loss that occurs with aging. Secondary osteoporosis is a result of medications (e.g., glucocorticoids) or diseases (e.g., malabsorption) that adversely affect skeletal health.
FIGURE 1. Micrographs of Normal vs. Osteoporotic Bone 13
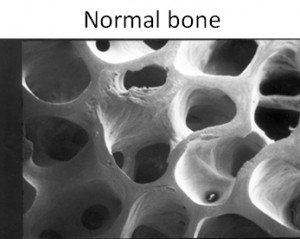
From: Dempster, DW et al., with permission of The American Society for Bone and Mineral Research.1,3
PREVALENCE IN WOMEN
Osteoporosis is responsible for an estimated 90% of all hip and spine fractures in white American women ages 65 to 84.12 For a white American woman at age 50, the risk of suffering an osteoporotic fracture in her remaining lifetime has been estimated at 40%, with two-thirds of the fractures occurring after age 75.12 In the United States osteoporosis and fracture vary by ethnicity.12 In one large study of postmenopausal women from five ethnic groups (white Americans, African Americans, Asian Americans, Hispanic Americans and Native Americans), African Americans had the highest bone mineral density (BMD) and Asian Americans had the lowest BMD. The BMD differences for African Americans were not explained by differences in weight. After adjusting for weight, BMD, and other variations, white American and Hispanic Americans had the highest risk of osteoporotic fracture, followed by Native Americans, African Americans, and Asian Americans.12
PREVALENCE IN MEN
One out of 4 men over 50 years old will have a bone fracture due to osteoporosis. The reasons why men do not develop osteoporosis as frequently as women are several. Firstly, men start puberty later than women and continue longer versus women; therefore they have a longer bone maturation period. Secondly testosterone in men during puberty leads to development of larger skeletons, where as estrogen in women does not. Lastly, testosterone may increase bone mass, however, estrogen conserves bone mass.
RISK FACTORS
There are several risk factors that predispose one to developing osteoporosis. They are advanced age, female sex, genetics, lifestyle factors (such as low dietary intake of calcium and vitamin D, smoking),thinness,and menopause status. The greatest influence on a woman’s peak bone mass (the maximal BMD gained during the skeletal development and maturation phase) is heredity. Studies have suggested that up to 80% of the variability in peak BMD might be attributable to genetic factors.12 Daughters of women who have osteoporotic fractures have lower BMD than would be expected for their age.12 Furthermore, a history of fracture in a first degree relative also significantly increases the fracture risk. Hip fracture risks were from 50% to 127% higher if a hip fracture had occurred in a parent12.
There are also disease states and drugs that can increase the risk of osteoporosis. A summary of risk factors is shown in Table 1.Primary causes of osteoporosis are those one has little control over, but secondary causes one can modify to reduce risk.
TABLE 1 Risk Factors for Osteoporosis
| Primary | Secondary |
|---|---|
| Gender | Medications |
| Age | Diseases |
| Body size | Calcium and Vitamin D Intake (low) |
| Ethnicity | Sex Hormone level (low) |
| Family History | Anorexia Nervosa |
| Smoking | |
| Excessive alcohol intake | |
| Activity level |
Some medicines are harmful to bones12(Table 2).Talk to your health care provider to take the necessary supplements to prevent or reduce the bone loss.
| The following medicines may cause bone loss: |
Table 2
- Antacids that have aluminium in them
- Some antiseizure medicines like Dilantin®, Phenobarbital
- Arimidex®, Aromasin® and Femara® that are caleed aromatase inhibitors
- Chemotherapeutic drugs like Cyclosporine A and FK506 (Tacrolimus), Methotrexate
- Gonadotropin releasing hormone (GnRH) such as Lupron® and Zoladex®
- Anticoagulating agent like Heparin
- Lithium
- Medroxyprogesterone (Depo-Provera®)for contraception
- Proton pump inhibitors (PPIs) such as Nexium®, Prevacid® and Prilosec®
- Selective serotonin reuptake inhibitors (SSRIs) like Lexapro®, Prozac® and Zoloft®
- Steroids (glucocorticoids) e.g. cortisone and prednisone
- Tamoxifen® (premenopausal use)
- Thiazolidinediones e.g. Actos® and Avandia®
Note: This list may not include all medicines that may cause bone loss.
HOW DO YOU KNOW IF YOU HAVE OSTEOPOROSIS?
Osteoporosis can be clinically diagnosed, however, it has no warning signs. Often, the first indication of the disease is a fracture. Nearly all-nonvertebralfractures are caused by a fall; however, vertebral fractures often occur without a fall, and need not necessarily be painful. Only roughly one third of vertebral fractures are painful, and two thirds are painless. Marked height loss or kyphosis (severely stooped posture) over the years may be a sign of underlying vertebral compression fractures, even without significant associated back pain. Wrist or other fractures may occur at a younger age than vertebral or hip fractures and may also be early clinical signs of osteoporosis. Bone strength (and, hence, fracture risk) is dependent on many qualities of bone, of which bone mineral density (BMD) is the most commonly measured.6 Expressed, as grams of mineral per area or volume, BMD at any given age is a function of both peak bone mass (reached by age 30) and how much bone is subsequently lost.The most widely recognized BMD test is a dual-energy x ray absorptiometry, or DXA test. The test is painless – similar to having an x ray, but with much less exposure to radiation. It can measure bone density at your hip and spine. A BMD test can identify the following:(1) osteoporosis before a fracture occurs, (2)confirm a diagnosis of osteoporosis if you already have one or more fractures, (3)determine your risk for future fractures, and (4)measure your response to osteoporosis treatment.
Guidelines from the National Osteoporosis Foundation and Endocrine Society recommend testing bone density in all women age 65 and older, plus men who are 70 years of age and older.9The following risk factors should also prompt BMD testing earlier in men and women ages 50 – 69: alcohol abuse, chronic corticosteroids, celiac disease, diabetes, family history of osteoporotic fracture, previous fall or fracture, hypogonadism, smoking, and thinness. There are also recommendations for when spinal imaging should be performed.12
PREVENTION
The National Osteoporosis Foundation (NOF) has universal recommendations for the general population as follows:
- Lifelong participation in regular weight bearing and muscle strengthening exercises
- Stop smoking
- Reduce alcohol intake, treatment for alcoholism
- Lifelong adequate dietary intake of calcium and supplementation ifdietary intake is not enough
- Identify and treat risk factors for falling
NOF supports Institute of Medicine (IOM) recommendations that men age 50-70 consume 1,000 mg per day of calcium and that women age 51 and older plus men age 71 and older consume 1,200 mg per day of calcium.There is no evidence that calcium intake in excess of these amounts leads to additional bone strength. Intakes in excess of 1,200 to 1,500 mg per day may increase the risk of developing kidney stones, cardiovascular disease and stroke. The scientific literature is highly controversial in this area.12
CALCIUM SUPPLEMENTS
When it comes to calcium supplements, calcium carbonate (Caltrate, Tums) is the most cost effective and provides the most elemental calcium by weight. Absorption is better with food. Calcium citrate is a better choice for those with low gastric acidity10(elderly, those taking stomach acid reducing meds). It is better absorbed than calcium carbonate, however, to get the same amount of calcium more tablets are needed. It is also better absorbed on an empty stomach. There are other calcium salts available over the counter: calcium gluconate, calcium lactate, calcium glucarate, and calcium glubionate. These other formulations have much less elemental calcium so the only reason one should be selected over calcium carbonate or citrate is that they are available in chewable tablet, powder and liquid form for those patients who cannot or prefer not to take tablets. Watch out for supplements derived from coral and dolomite (a type of limestone) because these may contain lead and other heavy metals. Lead content in oyster shell, bone meal and other refined calcium products is considered to be safe10. Several calcium products are combined with Vitamin D. Vitamin D plays a major role in calcium absorption, bone health, muscle performance, balance and risk of falling12. NOF recommends an intake of 800 i.u. (Internationalunits) to 1000 i.u of Vitamin D for adults 50 and older. The addition of magnesium and vitamin K to calcium supplements are becoming more popular. Vitamin K is increasingly thought to have a role in bone health. It is thought to promote bone formation and reduce calcium excretion. 10Preliminary studies suggest that low vitamin K levels are related to fracture risk10. For those taking warfarin, most doctors agree that in most cases calcium with vitamin k does not need to be avoided as long as the supplement is taken consistently and the person managing the dosing is aware of it.
Magnesium deficiency increases the formation and activity of osteoclast (the bone cells involved in bone reabsorption)10. It may improve bone mineral density and be theoretically beneficial for osteoporosis. It does not increase calcium absorption as popularly believed, however, the laxative effect may help prevent constipation due to calcium ingestion. For most people single ingredient calcium supplements are fine, unless you know you are vitamin D deficient. If that is the case then a supplement with vitamin D is better.
TREATMENT
As has been discussed previously, osteoporosis can be prevented, diagnosed and treated before fractures occur. Importantly, even after the first fracture has occurred, there are effective treatments to decrease the risk of further fractures. The criteria to treat are the same in men 50 years old as it is in postmenopausal women9. After treatment is initiated BMD testing should be performed with a DEXA test every one to 2 years12.
| Suggestions For Making Your Living Space Safe From Falls (Figure 3) |
A comprehensive treatment program includes addressing proper nutrition, exercise, and safety issues to prevent falls. In regards to safety issues a medication review is needed to identify any drugs that may be contributing to falls due to drowsiness or dizziness. It is important that individuals with osteoporosis be aware of any physical changes that affect their balance or gait, and that they discuss these changes with their health care provider. Furthermore, it is recommended to perform an inspection of one’s house and yard to eliminate obstacles, throw rugs, etc. that can lead to tripping. Installation of grab bars, or use of stabilizing devices like canes and walkers should be considered if instability is an issue. Figure 3 provides tips to help eliminate the environmental factors that lead to falls.
OUTDOORS
- Use a cane for added stability
- Wear rubber-soled shoes for traction.
- Walk on grass when sidewalks are slippery.
- In winter, carry salt or kitty litter to sprinkle on slippery sidewalks
- Be careful on highly polished floors that become slick and dangerous when wet
- Use plastic or carpet runners when possible
INDOORS
- Keep rooms free of clutter, especially on floors.
- Keep floor surfaces smooth but not slippery
- Wear supportive,low-heeled shoes even at home.
- Avoid walking in socks, stockings, or slippers
- Be sure carpets and area rugs have skid-proof backing or are tacked to the floor.
- Be sure stairwells are well lit and that stairs have handrails on both sides.
- Install grab bars on bathroom walls near tub, shower and toilet
- Use a rubber bath mat in shower or tub.
- Keep a flashlight with fresh batteries beside your bed.
- If using a step stool for hard-to-reach areas, use a sturdy one with a handrail and wide steps.
- Consider purchasing a cordless phone so that you don’t have to rush to answer the phone when it rings, or so that you can call for help if you do fall.
MEDICATIONS[*]
Several FDA approved drugs are available for prevention and/or treatment of osteoporosis. The following section sumerizes current options.
- Bisphosphonates:( Fosamax, Boniva, Actonel, Recast): There are oral and injectable formulations and they have a range of dosing frequencies (daily, weekly, monthly). The injectable formulations are given either every 3 months or once yearly. Bisphosphonates are first line choice for most people to prevent or treat osteoporosis. They have gastrointestinal side effects: esophagitis, upset stomach, diarrhea, heartburn, and difficulty in swallowing. The oral dosage forms must be taken first thing in the morning on an empty stomach with 8 ounces of water and one needs to remain upright for at least 30 minutes after taking dose.
- Estrogen (ET)/hormone therapy (HT): ( [ET] Climara, Estrace, Estraderm, Ogen, Premarin, Vivelle) ([HT]: Femhrt, Prempro) ET/HT dosages include cyclic, sequential and continuous regimens. If and when treatment is stopped, bone loss can be rapid and alternative agents should be considered to maintain BMD. Because of the increased risk of stroke, breast cancer, and blood clots, other non-estrogen drugs should be considered first if used solely to prevent osteoporosis.
- Estrogen Agonist/antagonist :(Evista, Fareston) Taken daily for treatment and prevention of osteoporosis. Raloxifene (Evista) is also indicated for the reduction in risk of invasive breast cancer in postmenopausal women with osteoporosis.Raloxifene increases the risk of deep vein thrombosis to a degree similar to that observed with estrogen. It can also increase hot flashes and cause leg cramps.
- Conjugated estrogens combined with estrogen agonist/antagonist : (Duavee) The medication combines conjugated estrogen with an estrogen agonist/antagonist (bazedoxifene). The bazedoxifene component reduces the risk of endometrial hyperplasia (excessive growth of the lining of the uterus) that can occur with the estrogen component of the drug. Therefore progestins do not need to be taken with conjugated estrogens/bazedoxifene. Duavee is taken daily without regard to meals and carries the same risks as above with hormone therapy.
- Parathyroid hormone: (Teriparatide – Forteo) For postmenopausal women and men at high risk of fracture due to drug induced osteoporosis due to glucocorticoid (Prednisone) therapy. It is a bone building agent administered subcutaneously every 6 months by a health professional. It can cause leg cramps, nausea, and dizziness. Treatment should not exceed 18 – 24 months and is commonly followed with a bisphosphonate to maintain or further increase BMD.12
- RANKL Inhibitor: Denosumab (Prolia) For postmenopausal women at high risk of fracture and to treat bone loss in women with breast cancer on aromatase inhibitor therapies (i.e. Tamoxifen) and bone loss in men with prostate cancer taking gonadotropin-reducing hormone therapy (i.e. Lupron) and are at high risk for fracture. It is given as a subcutaneous injection by a health professional every 6 months. It can cause hypocalcemia (low calcium) and increased risk of serious skin infections (cellulitis) and skin rash.
CONCLUSION
Osteoporosis is mostly a bone disease of aging. Most women and men do not have to worry about it until the 5thdecade of life. It is firstly important to prevent osteoporosis by reducing or eliminating controllable risk factors such as smoking, inactivity, excessive alcohol intake and lack of calcium in the diet. Secondly, addressing and fixing fall risks in your home environment cannot be emphasized enough. Ask your physician about your concerns regarding osteoporosis, so you both can do as much as possible to prevent osteoporosis initially, or keep it from becoming worse.
[*] Drug information is abbreviated and not complete
REFERENCES
- “National Institutes of Health Osteoporosis Overview.” U.S National Library of Medicine. U.S. National Library of Medicine, Jan. 2012. Web. 23 Apr. 2015. <http://nih.gov/>.
- Roldan, MD, Carlos J., and Linda Paniagua, MD. “Complications of New Medications.” West J Emerg Med 16.1 (2015): 154-56. Print.
- Coluzzi, Flaminia, Joseph Pergolizzi, Robert B. Raffa, and Consalvo Mattia. “The Unsolved Case of “bone-impairing Analgesics”: The Endocrine Effects of Opioids on Bone Metabolism.” Therapeutics and Clinical Risk Management 11 (2015): 515-23. Print.
- Willson, Tina, Scott D. Nelson, Jonathan Newbold, Richard E. Nelson, and Joanne LaFleur. “The Clinical Epidemiology of Male Osteoporosis: A Review of the Recent Literature.” Clinical Epidemiology 7 (2015): 65-76. Print.
- Morsy Elsisi, Hany Farid Eid, Gihan Samir Mohamed Mousa, and Mohamed Taher Mahmoud Eldesoky. “Electromagnetic Field versus Circuit Weight Training on Bone Mineral Density in Elderly Women.” Clinical Interventions in Aging 10 (2015): 539-48. Web.
- PL Detail-Document, Comparison of Medications for Osteoporosis. Pharmacist’s Lett/Presciber’s Letter. July 2012
- PL Detail-Document, Optimal Duration of Bisphosphonate Therapy. Pharmacist’s Letter/Prescriber’s Letter. July 2013
- PL Detail-Document, Managing Suboptimal Response to Bisphosphonates. Pharmacist’s Letter/Prescriber’s Letter. October 2013
- PL Detail-Document, Osteoporosis in Men. Pharmacist’s Letter/Prescriber’s Letter. September 2012.
- Comparison of oral calcium salts. Pharmacist’s Letter/Prescriber’s Letter 2008;24(10):241008.
- &na;. “Management of Osteoporosis in Postmenopausal Women.” Menopause1 (2010): 25-54. Web.
- National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. April 1,2014.http://nof.org/files/nof/public/content/file/2791/upload/919.pdf (accessed May 14,2014).